发布时间:2021年02月26日 08:36:58 来源:振东健康网
编辑翻译:菁菁
译文校对:奇奇
本报告于2021年2月首次发表在最新的JACC病例报告库,为多学科团队直播案例。报告介绍了多学科团队处理医源性主动脉冠状动脉夹层的过程和诊断细节。
1、摘要
本文介绍一例医源性主动脉冠状动脉夹层处理案例。该患者因稳定型心绞痛接受常规经皮冠状动脉介入治疗(PCI),其治疗过程中发生了医源性主动脉冠状动脉夹层。真内腔和支架植入物应仔细缝合以封闭剥离皮瓣,防止急性并发症。基于计算机断层扫描主动脉造影,本案例中采用保守方法处理残留的主动脉夹层。(难度级别:中级。)
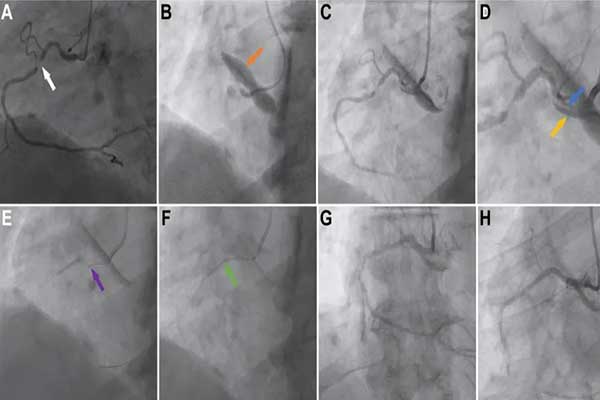
图注:(A)基线诊断性血管造影显示病变前的牧羊杖弯曲(白色箭头)。(B)最初的衔接和测试注射产生了主动脉冠状动脉夹层(橙色箭头)。(C)非选择性血管造影显示,该切口低于右冠状动脉口,但最初保持血管向下流动。(D)切口放大图像显示,有假内腔(黄色箭头)和真内腔(蓝色箭头)。(E)将一根导引导丝(Balance Middle Weight Universal wire,Abbott Vascular,加利福尼亚州圣克拉拉)放入假内腔作为标记(紫色箭头),然后将一根金属丝(Sion Blue,Asahi Intecc,东京,日本)穿入右侧冠状动脉远端,以使病变部位扩张。(F)选择一个药物洗脱支架(Xience Sierra,Abbott Vascular)(绿色箭头)以覆盖病变并封闭剥离瓣。(G)和(H)在扩张后心肌梗塞溶栓治疗之后,右侧冠状动脉恢复了第3级血流,且症状、电生理和血流动力学得到改善。
2、简介
一位78岁的男性患者,此前身体健康,本次就诊时表现出劳累性胸痛,伴有稳定型心绞痛。该患者接受了最佳药物治疗,包括阿司匹林、阿托伐他汀、比索洛尔、单硝酸异山梨酯,但症状持续存在。他在另一个医学中心接受了诊断性血管造影。患者有高血压病史,没有其它冠心病相关的危险因素。诊断性血管造影显示,在“牧羊杖”型近端径向翘起(图1A)之外,右侧近端冠状动脉严重狭窄(图1A)。另一个医学中心的经胸超声心动图检查显示心脏结构正常。考虑到他的持续症状和诊断性血管造影严重狭窄,选择了RCA的选择性经皮冠状动脉介入治疗(PCI)。
现有多种方法可以治疗该疾病。先前的诊断性血管造影显示近端RCA有牧羊杖状弯曲,并出现严重的内膜钙化。这一发现表明,气球和支架植入难度较高。预先考虑到这一情况,医师选择了Amplatz(Medtronic,明尼阿波利斯,明尼苏达州)左0.75导尿管,因为它提供了比Judkins(Medtronic)右4.0导尿管更好的被动支撑。Judkins(Medtronic)是英国剑桥皇家帕普沃斯医院的标准RCA导尿管。替代策略包括使用支撑力较小的引导器但使用导线支撑器,或引导导管延伸以输送设备。
使用6-F鞘管从右侧桡动脉进入。根据近端 RCA的曲折度,选择了Amplatz左0.75导尿管,以确保良好的被动导尿管支持。尽管接合没有特别困难,但最初的测试注射显示导管引起的主动脉切开,恰好在RCA口下方(图1B)。非选择性进样显示了切开后RCA中的残留流量(图1C和1D)。
3、结论
引导导管诱发的主动脉冠状动脉夹层是公认的PCI并发症,操作者应对有危险因素的患者保持警惕。在情况允许时,应对患有医源性冠状动脉夹层的患者立即植入支架。横截面成像结果对于判断选择心脏手术或保守治疗至关重要。
英文原文
Iatrogenic Aortocoronary Dissection During Percutaneous Coronary Intervention: Investigation and Management
1. Abstract
We present a case of iatrogenic aortocoronary dissection sustained during routine percutaneous coronary intervention for stable angina. Careful wiring of the true lumen and stent implantation to seal off the dissection flap prevented immediate complications, and computed tomography aortography guided a conservative approach to manage the residual aortic dissection. (Level of Difficulty: Intermediate.)
2. Introduction
A 78-year-old man, previously fit and well, presented with exertional chest pain consistent with stable angina. He was treated with optimal medical therapy including aspirin, atorvastatin, bisoprolol, and isosorbide mononitrate, but his symptoms persisted, and he underwent diagnostic angiography at another center. His past medical history consisted of hypertension with no other risk factors for coronary artery disease. Diagnostic angiography demonstrated severe stenosis in the dominant, proximal right coronary artery (RCA) beyond a “shepherd’s crook”–type take-off and a proximal course (Figure 1A). Transthoracic echocardiography at another center showed a structurally normal heart. Given his ongoing symptoms and severe stenosis on diagnostic angiography, he chose elective percutaneous coronary intervention (PCI) to the RCA.
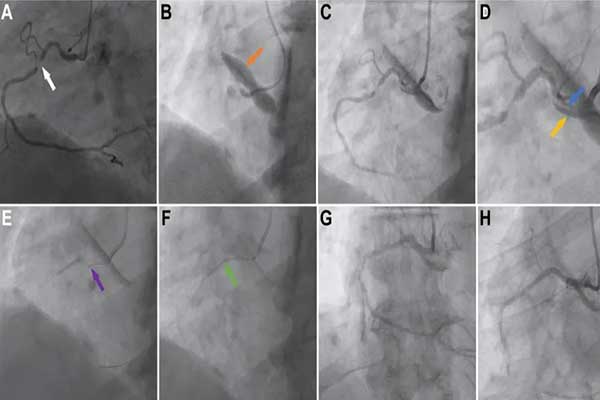
Angiographic Images of Dissection and Subsequent PCI
(A) The baseline diagnostic angiogram demonstrates shepherd’s crook anatomy before the lesion (white arrow). (B) Initial engagement and test injection produced an aortocoronary dissection (orange arrow). (C) Nonselective angiography showed that the dissection was inferior to the right coronary artery ostium, but initially flow down the vessel was maintained. (D) An enlarged image of the dissected ostium is shown with the false lumen (yellow arrow) and the true lumen (blue arrow). (E) A Balance Middle Weight Universal wire (Abbott Vascular, Santa Clara, California) was placed in the false lumen as a marker (purple arrow), and a Sion Blue (Asahi Intecc, Tokyo, Japan) wire was passed to the distal right coronary artery to allow ballooning of the lesion. (F) An Xience Sierra drug-eluting stent (Abbott Vascular) (green arrow) was selected to cover the lesion and also to seal the dissection flap. (G) and (H) After post-dilation Thrombolysis In Myocardial Infarction flow grade 3 was restored in the right coronary artery, with symptomatic, electrical, and hemodynamic improvement. PCI = percutaneous coronary intervention.
There are numerous approaches to treating this lesion. A previous diagnostic angiogram had already demonstrated a shepherd’s crook tortuosity in the proximal RCA with severe intimal calcification. This finding suggested that delivery of balloons and stents would be more challenging. Anticipating this situation, an Amplatz (Medtronic, Minneapolis, Minnesota) left 0.75 guide catheter was selected because it provides better passive support than a Judkins (Medtronic) right 4.0 catheter, which was the standard RCA guide catheter at Royal Papworth Hospital, Cambridge, United Kingdom. Alternative strategies included using a less supportive guide, but with the use of buddy wire support, or guide catheter extension to deliver equipment.
Access was obtained from the right radial artery with a 6-F sheath. An Amplatz left 0.75 guide catheter was selected on the basis of the tortuosity of the proximal RCA, to ensure good passive guide support. Although there was no particular difficulty in engagement, the initial test injection demonstrated catheter-induced dissection of the aorta, just below the RCA ostium (Figure 1B). A nonselective injection demonstrated residual flow in the dissected RCA (Figures 1C and 1D).
3. Conclusions
Guide catheter–induced aortocoronary dissection is a recognized complication of PCI, and operators should remain vigilant in patients with risk factors. Iatrogenic coronary dissection should usually be managed by immediate stent implantation when possible, and cross-sectional imaging is essential to decide whether cardiac surgery or a conservative strategy is most appropriate for the ascending aorta.
