发布时间:2021年04月14日 08:44:53 来源:振东健康网
编辑翻译:菁菁
译文校对:奇奇
本报告在2021年4月最新的医学学术期刊《泌尿病例报告》(Urology Case Reports)首次刊发,报告关注了一位同时患有黄色肉芽肿性前列腺炎,前列腺癌和前列腺脓肿的患者,介绍了诊疗过程。
1、摘要
黄色肉芽肿性前列腺炎(XGP)是一种罕见的疾病,有时与前列腺癌的影像结果和临床表现非常相似。鉴别这一疾病对采用正确的治疗方式至关重要。前列腺组织的组织学检查能够确切地将XGP与前列腺癌区分开。该病例罕见地同时存在前列腺脓肿、前列腺癌、XGP,后续诊断则模糊不清。经皮穿刺抽吸术和针对脓肿的抗生素治疗缓解了下尿路症状,并在随后的前列腺活检中消除了XGP。必须认真进行检查,以避免不必要的干预或漏诊。
2、简介
黄色肉芽肿性前列腺炎(XGP)是一种罕见的组织学诊断。前列腺组织中含有黄色瘤或富含胆固醇,且存在特发性肉芽肿性前列腺炎。目前,文献中报告的该疾病病例不到20例。这一疾病的常见临床表现包括下尿路症状(LUTS)、骨盆疼痛和检查时可触及的结节,通常在60至70岁人群中诊断出。在进行经尿道前列腺电切术时,XGP也与前列腺脓肿有关。
该疾病的组织学特征是巨噬细胞充满脂质,称为“泡沫组织细胞”,有巨细胞、淋巴细胞、纤维素增生。免疫组织化学检查结果显示CD68(+)、PSA(-)。CD68(+)对于描述与疾病相关的黄色瘤十分重要。当与XGP结合时,前列腺通常会肿大,质量范围通常在50-60g内。当前的PSA是不断变化的,变化范围为0.5到172 ng / dL。在PSA明显升高> 150 ng / dL的患者中,PSA的水平在手术治疗后4个月开始下降,在切除后17个月降至6 ng / dL。
一位65岁的男子最近被诊断出患有2型糖尿病,该患者被感染的左肩关节呈现金黄色葡萄球菌(MSSA)菌血症,对甲氧西林敏感。患者陈述患有糖尿病性酮症酸中毒,多脓毒性空化肺栓塞和多器官衰竭。患者尿液培养对MSSA呈阳性。腹部和骨盆的CT显示,在AP平面上有一个2.6×2.6 cm的偏心小叶直肠肿块。在进行柔性乙状结肠镜检查和可疑直肠肿块活检时,咨询了肠胃科。在内镜检查过程中,发现直肠附近有一个外部肿块(图1A),并进行了活检。活检证实直肠增生粘膜。在内镜超声检查中,发现有一个 3.7×3.0 cm的病灶,其起源似乎是前列腺(图1B)。由于担心癌症播种,医师决定不进一步对肿块进行活检。
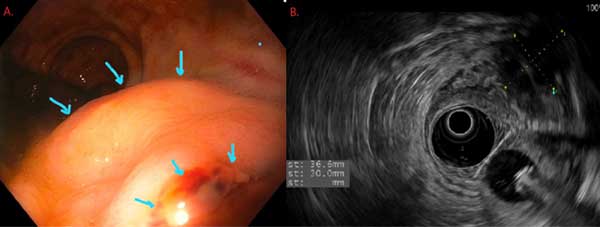
图1. A.乙状结肠镜检查显示,有覆盖直肠粘膜的外部肿块。 B.内窥镜超声检查显示,有固体和液体成分的前列腺组织
经泌尿科评估,患者下尿路症状包括夜尿、尿滴沥、排尿困难、尿不尽。该患者PSA为1.23ng/mL,其他泌尿科病史为曾经患有肾结石,没有肾脏、前列腺、膀胱相关癌症的个人或家族病史。检查时,他的前列腺无触痛,估计重40克,并显示出明显的左侧结节。
患者临床稳定且接受抗生素治疗数天后,接受了前列腺穿刺活检。前列腺经直肠超声检查发现有低回声区,与患者积液位置一致。使用一根18号规格的脊椎针排出积液后进行了活检,包括标准12芯活检和3芯可疑结节活检。
前列腺穿刺活检的病理结果表明,在几个核芯中均出现了黄褐质性瓣膜性前列腺炎,在单个核芯中有5%的患者出现了格里森3+4=7前列腺腺癌(图2A和B)脓肿的前列腺液培养与金黄色葡萄球菌一致,随后用达托霉素进行处理。
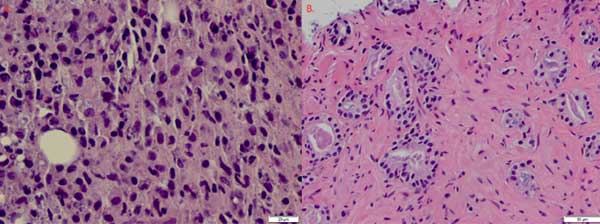
图2. A.泡沫组织细胞的组织病理学特征表明有XGP。B.组织病理学表现出格里森3+4=7前列腺腺癌
中度风险前列腺癌的主动监测显示,患者的症状(包括排尿困难)有所改善。大约在初次住院后8个月,再次进行前列腺活检。检查显示,在以前的癌症区域,在标准的12个核芯和4个额外的活检组织中发现了良性前列腺组织。
3、讨论
据我们所知,这是首次报告一位患者同时患有XGP、前列腺脓肿和前列腺癌。黄色肉芽肿性疾病在肾脏中最为常见,但在一些罕见病例中,能够在胆囊和前列腺中观察到该疾病。在XGP中,已经报告了各种LUTS。检查时,通常会接触前列腺结节。像在肾脏中一样,前列腺中黄色肉芽肿性疾病的成像结果具有欺骗性和非特异性。虽然本例患者的PSA水平正常,但先前的病例报告中该水平通常升高,这意味着与正常的前列腺癌(成像结果)相似,进一步混淆了初期诊断。
更罕见的是在患有XGP的情况下同时患有前列腺脓肿。此前,文献中记载的病例只有五例。我们的报告强调了在患者患有前列腺癌和前列腺脓肿的背景下诊断出XGP的可能性,这使诊断更加复杂。因此,该病例启示,需要密切注意组织病理学和其他并发疾病,例如前列腺脓肿,以确保准确的诊断和治疗。如本例所示,采用引流术和抗生素成功治疗了脓肿和XGP。尽管临床表现容易与前列腺癌混淆,这一疾病也可与前列腺癌同时出现。
4、结论
XGP是一种罕见的临床诊断,可能与前列腺脓肿有关。众所周知,XGP的成像结果和临床表现与前列腺癌类似。本文介绍了一例罕见病例,患者PSA正常,但患有XGP,前列腺脓肿,以及前列腺癌。该患者成功接受了引流、抗生素治疗,并接受了积极监测。
英文原文
An improbable trifecta: Occurrence of xanthogranulomatous prostatitis, prostate cancer, and prostatic abscess in a single patient
1、Abstract
Xanthogranulomatous prostatitis (XGP) is a rare disease that can mimic the clinical and imaging findings of prostate cancer. Differentiation of these diseases is vital in order to offer the correct treatment. Histological examination of prostate tissue is the definitive manner in which XGP is distinguished from prostate cancer. This case demonstrates the rare possibility of concurrent findings of prostate abscess, prostate cancer, and XGP, further clouding diagnostic assessment. Percutaneous aspiration and antibiotic treatment of the abscess reduced lower urinary tract symptoms and eliminated XGP on subsequent prostate biopsy. Careful work up is necessary to prevent unnecessary interventions or missed diagnoses.
2、Introduction
Xanthogranulomatous prostatitis (XGP) is a rare histological diagnosis comprised of prostate tissue that contains xanthomas, or cholesterol laden histiocytes, along with idiopathic granulomatous prostatitis. There are currently fewer than 20 reported cases in the literature. Common clinical manifestations of the disease include lower urinary tract symptoms (LUTS), pelvic pain, and palpable nodule on exam, with a diagnosis typically in the 6th decade of life. It has also been associated with prostatic abscess at the time of transurethral resection of the prostate.
The disease has histologically been characterized by lipid-laden macrophages, or “foamy histiocytes,” with giant cells, lymphocytes, and fibroplasia. Characterization of the disease via immunohistochemistry shows CD68 (+) and PSA (−). CD68 (+) is important for describing the xanthomas associated with the disease. The prostate is often enlarged when associated with XGP, typically with a mass in the range of 50–60g. The presenting PSA is variable, ranging from 0.5 to 172 ng/dL. In those with significant elevations in PSA >150 ng/dL, decline in the PSA levels began 4 months after surgical treatment and decreased to 6 ng/dL 17 months after resection.
3、Case presentation
We present an interesting case of a 65 year old man with recently diagnosed diabetes mellitus type 2 who presented with Methicillin-sensitive Staphylococcus aureus (MSSA) bacteremia from an infected left shoulder joint. At presentation, he suffered from diabetic ketoacidosis, multiple septic cavitary pulmonary emboli, and multiorgan failure. His urine culture was positive for MSSA. CT of the abdomen and pelvis demonstrated an eccentric lobular rectal mass measuring 2.6 ×2.6 cm in AP plane. Gastroenterology was consulted for flexible sigmoidoscopy and biopsy of the suspected rectal mass. During endoscopy, they noted an external mass adjacent to the rectum (Fig. 1A), which was biopsied. This biopsy demonstrated hyperplastic rectal mucosa. On endoscopic ultrasound, they noted a 3.7 × 3.0 cm lesion that appeared prostatic in origin (Fig. 1B). Due to concern for cancer seeding, they elected not to further biopsy the mass.
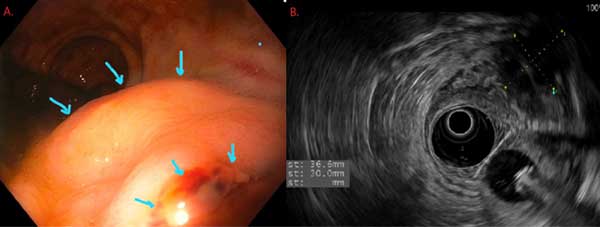
Fig. 1. A. Sigmoidoscopy showing an external mass with normal overlying rectal mucosa. B. Endoscopic ultrasound demonstrating a prostate mass with solid and liquid components.
Upon urologic evaluation, the patient reported baseline LUTS including nocturia, as well as weak stream, hesitancy, and incomplete emptying. His PSA was 1.23 ng/mL. Other urologic history included a previous spontaneous passage of a renal stone. He had no personal or family history of kidney, prostate, or bladder cancer. On exam, his prostate was non-tender, estimated at 40g, and demonstrated a palpable left sided nodule.
After the patient had clinically stabilized and had been on antibiotics for several days, the patient was offered a prostate biopsy. On transrectal ultrasound of the prostate there was a hypoechoic area consistent with abscess fluid. An 18 gauge spinal needle was used to drain seropurulent fluid which was sent for culture. Biopsies were taken including the standard 12 core biopsy and 3 cores of the suspicious nodule.
Pathology from the prostate biopsy demonstrated xanthogranulom atous prostatitis in several cores, as well as Gleason 3 + 4 = 7 prostate adenocarcinoma in 5% of a single core (Fig. 2A and B). Prostatic fluid culture from the abscess was consistent with Staphylococcus aureus, which was subsequently treated with Daptomycin.
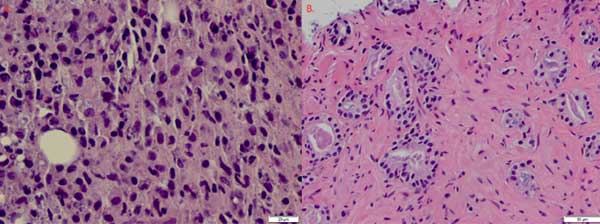
Fig. 2. A. Histopathology showing foamy histiocytes demonstrating XGP.B. Histopathology showing Gleason 3 +4 =7 adenocarcinoma of the prostate
The patient’s symptoms, including dysuria, had improved. He elected for active surveillance of his favorable intermediate risk prostate cancer. Approximately 8 months after the original hospitalization a repeat prostate biopsy demonstrated benign prostatic tissue in the standard twelve cores and four extra biopsies taken in the previous area of cancer.
4、Discussion
To our knowledge, this is the first case report that demonstrates concomitant XGP, prostate abscess, and prostate cancer in the same patient. Xanthogranulomatous disease is most commonly recognized in the kidney, but has been observed in rarer cases in the gallbladder and prostate. In XGP, varying LUTS have been reported. On exam, a prostatic nodule is commonly palpated. As in the kidney, imaging may be deceptive and non-specific for xanthogranulomatous disease in the prostate. While the patient in our case had a normal PSA level, prior case reports have highlighted elevated levels, mimicking possible prostate cancer and further clouding the initial diagnosis.
Even more uncommon is the concurrent presentation of a prostate abscess in the setting of XGP, with as few as five cases documented in the literature prior to this. Our case highlights the possibility of XGP diagnosed in the setting of prostate cancer and prostate abscess, which further complicates the diagnosis. Therefore, this case stresses the need to pay close attention to the histopathology and any other concurrent disease, such as prostate abscess, in order to ensure accurate diagnosis and treatment. Conservative treatment with antibiotics and drainage, as in this example, successfully treated the abscess and XGP on subsequent biopsy. While the clinical presentation can be confused with prostatic adenocarcinoma, the two diagnoses can also co-exist.
5、Conclusion
XGP is a rare diagnosis that can be associated with prostate abscess. XGP has been known to mimic prostate cancer on imaging and in clinical presentation. We present a very rare case of a patient with normal PSA who was found to have XGP, prostate abscess, and prostate cancer. The patient was successfully treated with aspiration drainage, antibiotics, and was placed on active surveillance.
