发布时间:2021年07月28日 09:16:49 来源:振东健康网
资讯来源:University of Geneva
编辑翻译:奇奇
本文献于2021年7月发表在美国著名医学期刊《科学免疫学》(Science Immunology)。科学家们发现有些免疫反应机制相似,但是产生这些反应的细胞群不同,这为开发出更加有效且更加安全的癌症免疫疗法指明了方向。
最近几年,免疫疗法已经彻底改变了癌症治疗领域。然而,健康组织中的炎症反应经常会引发严重的副作用,并导致癌症治疗的永久终止。然而我们对该副作用依然所知甚少,这成了采用免疫治疗的一个主要障碍。
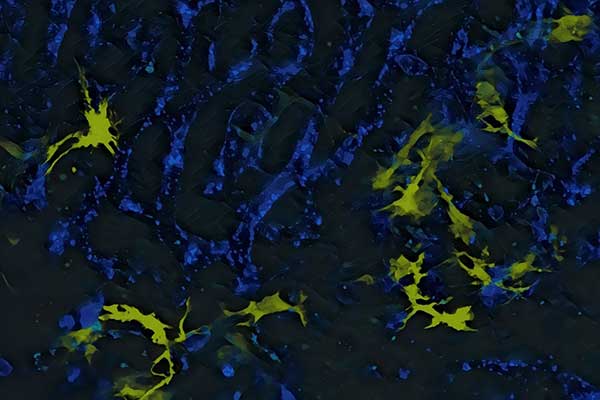
图片黄色区域:肝脏巨噬细胞或枯氏细胞,分泌IL-12蛋白,导致免疫治疗的不良反应。蓝色区域:血管。
来自瑞士日内瓦大学(UNIGE)和哈佛医学院的科学家们已经成功地确定了有害免疫反应和针对肿瘤细胞的免疫反应之间的区别。尽管两者的免疫机制相似,但它们所涉及的细胞群却不同。这项研究刊登在《科学免疫学》杂志上,可能会给患者带来更有针对性、更加有效果并且更低危险性的治疗方法。
基于对患者免疫系统的大规模刺激,免疫疗法已经挽救了许多生命。但不幸的是,它们并非没有副作用。Mikaël Pittet是UNIGE医学院病理免疫学和肿瘤血液学转化研究中心ISREC基金会主席,也是瑞士莱曼癌症中心成员。他说:“当免疫系统被强烈地激活时,由此导致的炎症反应会产生有害影响,有时还会对健康组织造成重大损害。因此,我们想要了解,旨在消除癌症的预期免疫反应和影响健康组织的不良反应之间是否有区别。识别出这两种免疫反应之间的独特成分,有助于开发出新的、更有效的、毒副作用更小的治疗方法。”
通过利用在CHUV和HUG经历过这种毒副作用反应治疗的病人的肝脏活检样本,科学家们研究了起作用的细胞和分子机制,来揭示相似性和不相似性。
不同细胞群的相似反应
在免疫治疗相关的毒副作用反应中,两种类型的免疫细胞(巨噬细胞和中性粒细胞)似乎负责攻击健康组织,但不参与杀死癌细胞。相比之下,另一种细胞类型(树突状细胞群)不攻击健康组织,但对于消除癌细胞却至关重要。
Pittet解释说:“免疫疗法可以触发特殊蛋白质的产生,这些蛋白质向免疫系统发出警报,并引发炎症反应。在肿瘤中,这些蛋白质是受欢迎的,因为它们允许免疫系统摧毁癌细胞。然而,在健康组织中,这些相同蛋白质的存在会导致健康细胞的破坏。实际上,这些炎症蛋白是由肿瘤和健康组织中的不同细胞产生的,这是一个有趣的发现。”
树突状细胞非常罕见,而巨噬细胞和中性粒细胞则更为常见。一些巨噬细胞从胚胎发育阶段就存在于我们的大多数器官中,并在我们的一生中一直存在。与以往的观点相反,这些巨噬细胞不一定能抑制炎症,但在免疫疗法的刺激下,它们可以在其所在的健康组织中引发有害的炎症反应,这也解释了为什么毒副作用会影响不同的器官。
中和中性粒细胞的双重好处
当巨噬细胞被药物激活时,它们会产生炎症蛋白,蛋白反过来激活中性粒细胞,中性粒细胞执行毒副作用反应。Pittet说:“这为通过控制中性粒细胞来限制免疫疗法副作用提供了可能性。”
通过研究细胞活性受遗传工具调节的小鼠的免疫反应,研究小组证实了他们的发现。他们能够识别出一个用来消除这些副作用的漏洞。事实上,中性粒细胞会产生一些对毒副作用发展很重要的因子,包括可能成为治疗靶点的TNF-α。TNF-α抑制剂已经用于调节关节炎患者的免疫反应,也可能在癌症治疗中用于抑制免疫疗法期间中性粒细胞的毒副作用。
Pittet说:“此外,抑制中性粒细胞可能是一种更有效的抗癌方式。中性粒细胞除了引发毒副作用反应外,其中一些细胞还会促进肿瘤生长。因此,通过设法控制它们,我们能够获得双重好处:克服健康组织中的毒副作用和限制癌细胞的生长。”
英文原文
Paving the Way for Cancer Treatments With Fewer Side Effects
In recent years, immunotherapy has revolutionized the field of cancer treatment. However, inflammatory reactions in healthy tissues frequently trigger side effects that can be serious and lead to the permanent discontinuation of treatment. This toxicity is still poorly understood and is a major obstacle to the use of immunotherapy.
Scientists from the University of Geneva(UNIGE), Switzerland, and Harvard Medical School have succeeded in establishing the differences between deleterious immune reactions and those targeting tumor cells. While the immune mechanisms are similar, the cell populations involved are different. This work, published in the journal Science Immunology, could lead to better targeted, more effective, and less dangerous treatments for cancer patients.
Based on massive stimulation of the patient's immune system, immunotherapies have saved many lives. Unfortunately, they are not without consequences." When the immune system is activated so intensively, the resulting inflammatory reaction can have harmful effects and sometimes cause significant damage to healthy tissue," says Mikaël Pittet, holder of the ISREC Foundation Chair in Onco-Immunology at UNIGE Faculty of Medicine Department of Pathology and Immunology and Centre for Translational Research in Onco-Haematology, and a member of the Swiss Cancer Centre Leman." Therefore, we wanted to know if there are differences between a desired immune response, which aims to eliminate cancer, and an unwanted response, which can affect healthy tissue. The identification of distinctive elements between these two immune reactions would indeed allow the development of new, more effective and less toxic therapeutic approaches."
Using liver biopsy samples from patients treated at the CHUV and the HUG who had suffered such toxic reactions, the scientists studied the cellular and molecular mechanisms at work to reveal similarities and dissimilarities.
A similar response, but with different cells
In an immunotherapy-related toxic response, two types of immune cells—macrophage and neutrophil populations—appear to be responsible for attacking healthy tissue, but are not involved in killing cancer cells. In contrast, another cell type—a population of dendritic cells—is not involved in attacking healthy tissue but is essential for eliminating cancer cells.
"Immunotherapies can trigger the production of specialized proteins that alert the immune system and trigger an inflammatory response, explains Pittet. In a tumor, these proteins are welcome because they allow the immune system to destroy cancerous cells. In healthy tissue, however, the presence of these same proteins can lead to the destruction of healthy cells. The fact that these inflammatory proteins are produced by such different cells in tumors and healthy tissue is therefore an interesting finding."
Dendritic cells are very rare, whereas macrophages and neutrophils are much more common. Some macrophages are presentin most of our organs from embryonic development stages and remain there throughout our lives. Contrary to previous belief, these macrophages do not necessarily inhibit inflammation, but when stimulated by immunotherapies, they can trigger a harmful inflammatory response in the healthy tissue where they reside, thus explaining why toxicity can affect different organs.
Neutralizing neutrophils for a double benefit
When macrophages are activated by drugs, they produce inflammatory proteins. These in turn activate neutrophils, which execute the toxic reaction." This opens the possibility of limiting immunotherapy's side effects by manipulating neutrophils," says Pittet.
The research team confirmed their discovery by studying the immune reactions of mice whose cell activity was modulated with genetic tools. They were able to identify a loophole that could be exploited to eliminate these side effects. Indeed, neutrophils produce some factors that are important for the development of toxicity, including TNF-α, which could be a therapeutic target. TNF-α inhibitors are already used to modulate the immune response in people with arthritis and could perhaps be useful in the cancer setting to inhibit the toxic effects of neutrophils during immunotherapy.
"Furthermore, inhibiting neutrophils could be a more effective way to fight cancer: in addition to triggering atoxic response, some of these cells also promote tumor growth. Thus, by managing to control them, we could have a double beneficial effect: overcome the toxicity in healthy tissues, and limit the growth of cancerous cells," says Pittet.
参考文献
M. Siwicki el al.," Resident Kupffer cells and neutrophils drive liver toxicity in cancer immunotherapy," Science Immunology (2021).
