发布时间:2021年11月16日 08:58:12 来源:振东健康网
摘要
本文献于2021年11月9日发表在美国著名期刊《eLife》上。来自美国德克萨斯州的生物医学研究人员开发了一种可以检测免疫疗法对早期癌症患者治疗效果的模型,这有助于医生为患者匹配个性化治疗,减少不必要的治疗副作用。
研究人员开发了一种可以在治疗早期预测癌症患者是否会对免疫疗法产生反应的模型。该模型为医生提供了一种检测方法,利用医院扫描和实验室测试的现有信息,可以确定哪些人将在癌症治疗的早期阶段受益于免疫疗法。这将允许患者接受个性化治疗,并可以避免一些人因可能无效治疗而产生的副作用。
王志辉教授是美国德克萨斯州休斯顿卫理公会研究所医学数学研究副教授,也是该研究的第一作者和资深合著者。他说:“虽然免疫疗法已经改变了一部分癌症患者的生存率,但持久的治疗效果仍然只在少数人群中看到。数学模型可以定性或定量地辨别癌症中潜在的复杂生物和物理过程,有助于优化治疗方法。我们想展示标准的临床对策,例如通过扫描图像和组织活检分析,可以建立一个模型,以预测可能从免疫疗法中受益的人群。”
该团队专注于研究患者对一类称为免疫检查点抑制剂的免疫治疗药物的反应。他们设计了一个模型来确定患者开始检查点抑制剂治疗后相对肿瘤体积随时间的变化。肿瘤体积的变化受到免疫系统和癌细胞之间复杂的生物交互作用的影响。他们通过关注可以组合成一个方程的三个测量来简化这种交互作用:恶性肿瘤细胞的生长能力、免疫细胞在肿瘤环境中杀死癌细胞的能力以及基于检查点抑制剂免疫疗法的潜在有效性。
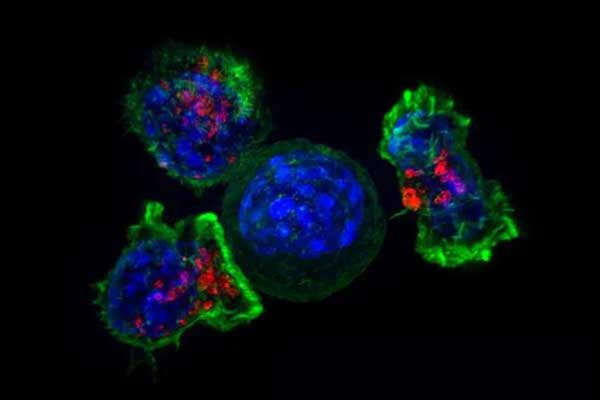
图注:杀伤性T细胞围绕着癌细胞。
绿色:杀伤性T细胞。蓝色:癌细胞。
他们首先使用临床试验的临床数据校准该模型,这些临床试验评估了一类专门针对PD-1/PD-L1通路的检查点抑制剂。试验测量了189名常见类型肿瘤患者的肿瘤体积随时间的变化。
然后,该团队将这个模型校准的结果与另外一组 64 名非小细胞肺癌患者的数据进行了比较,这些非小细胞肺癌患者接受了一种名为 Pembrolizumab(派姆单抗) 的免疫治疗药物。
他们发现,肿瘤环境中免疫细胞与肿瘤细胞的比例以及检查点抑制剂治疗的潜在有效性,在有反应的患者与无反应的患者之间都存在显着差异。重要的是,该模型仅使用肿瘤体积测量值就正确预测了81.4%的患者在治疗开始后两个月内发生的治疗反应。该模型在早期时间点(少于 60 天)预测反应的这种高灵敏度表明该模型可以为早期识别最有可能从检查点抑制疗法中受益的患者提供了有价值的信息。在预测从治疗中获益最少的患者组中,模型的假阴性结果也非常小。这对于确保模型正确预测患者从治疗中获益是很重要的。
“这里介绍的模型回顾性地研究了患者对免疫检查点抑制剂治疗的个体反应背后的分子、细胞和生物物理机制。我们已经证明,该模型可以可靠地利用来自常规扫描或组织活检分析的信息,而这些信息在治疗开始时就很容易获得。这些测量值可以作为个体患者早期使用免疫疗法治疗的有效性和准确指标。” 休斯顿德克萨斯大学MD安德森癌症中心放射肿瘤系副教授 Eugene Koay 总结道,他也是该研究的资深合著者。
英文原文
Model predicts early response to cancer immunotherapy
Researchers have developed a model that could predict early on in treatment whether cancer patients will respond to immunotherapy, according to a report published in eLife.
The model could provide doctors with a way to identify those who will benefit from immunotherapy at an early stage in their cancer treatment using readily available information from hospital scans and laboratory tests. This would allow patients to receive personalized treatment and could avoid some people experiencing side effects from a treatment that may not work for them.
"Although immunotherapy has transformed survival for a subset of cancer patients, durable treatment effects are still only seen in a minority," says Zhihui Wang, Associate Research Professor of Mathematics in Medicine, Houston Methodist Research Institute, Houston, Texas, US, and one of the co-first and co-senior authors of the study. "Mathematical models can qualitatively or quantitatively discern the underlying complex biological and physical processes in cancer which may otherwise be missed and can help optimize treatment approaches. We wanted to demonstrate how standard clinical measures, such as images from scans and analysis of tissue biopsies, could be used to build a model that predicts who might benefit from immunotherapy."
The team focused on looking at how patients respond to a class of immunotherapy drugs called immune checkpoint inhibitors. They designed a model to determine changes in relative tumor mass over time after patients start their checkpoint inhibitor therapy. The change in tumor mass is influenced by a complex biological cross-talk between the immune system and cancer cells. They simplified this cross-talk by focusing on three measurements that can be combined into an equation: The ability of malignant tumor cells to grow, the ability of immune cells to kill cancer cells within the tumor environment and the potential effectiveness of checkpoint inhibitor-based immunotherapy treatment.
They first calibrated this model using clinical data from clinical trials evaluating a class of checkpoint inhibitors that specifically target the PD-1/PD-L1 pathway. The trials measured changes in tumor volumes over time in 189 patients with common types of tumors.
The team then checked the results from this model calibration against data from an additional group of 64 patients with non-small cell lung cancer who were treated with an immunotherapy drug called pembrolizumab.
They found that the ratio of immune to tumor cells within the tumor environment, and the potential effectiveness of checkpoint inhibitor treatment, were both significantly different between responding versus non-responding patients. Importantly, the model correctly predicted the treatment response that occurred in 81.4% of patients using only tumor volume measurements and within two months of treatment initiation. This high sensitivity of the model to predict a response at early time points (less than 60 days) suggests that the model could provide valuable early identification of cancer patients most likely to benefit from checkpoint inhibition therapy. There were also minimal false-negative results from the model related to the group of patients predicted to receive the least benefit from therapy. This is important to ensure the model does not wrongly predict that a patient will not benefit from a treatment that might be effective.
"The model introduced here retrospectively investigates the molecular, cellular and biophysical mechanisms behind a patient's individual response to immune checkpoint inhibitor therapy," concludes Eugene Koay, Associate Professor at the Department of Radiation Oncology, University of Texas MD Anderson Cancer Center, Houston, and a co-senior author of the study. "We have demonstrated that this model can reliably use information from routine scans or tissue biopsy analysis, which are easily obtainable as early as the start of treatment. Together, these measurements may serve as early and accurate indicators of the effectiveness of immunotherapy treatment on an individual patient basis."
参考文献
Joseph D Butner et al, Early prediction of clinical response to checkpoint inhibitor therapy in human solid tumors through mathematical modeling, eLife (2021).
